+ General Considerations
- Insulinoma is usually an islet cell carcinoma of the pancreas
- Insulinoma is rare in cats (5 cases reported) and uncommon in dogs
- 60%-70% functional
- Hyperinsulinemia decreases glucose release from the liver by inhibiting hepatic enzymes responsible for gluconeogenesis and glycogenolysis
- Hyperinsulinemia decreases amino acid release from muscles and hence decreases the substrate for gluconeogenesis
- Decreased production of glucose is worsened by an increase in insulin-dependent uptake of glucose
- Hence, hyperinsulinemia results in hypoglycemia by decreasing glucose production and increasing glucose utilization
+ Signalment
- Mean age 9-10 years (range, 4-15 years)
- Breed predisposition: Irish Setter, Golden Retriever, German Shepherd Dog, Boxer, and Standard Poodle
- Insulinoma commonly affects medium to large breed dogs as 73% dogs are > 25 kg and 48% are > 35 kg
- No sex predilection
+ Clinical Signs
- Clinical signs are caused by hypoglycemia and resultant neuroglycopenia:
- Hypoglycemia due to increased insulin production by the tumor
- Catecholamine release secondary to hypoglycemia
- Common clinical signs include weakness and ataxia in the pelvic limbs, muscle tremors, dullness, disorientation, and decreased exercise tolerance
- Hypoglycemic convulsions or collapse are also common (67%)
- Type and severity of signs is determined by rate of glucose decline rather than absolute or relative glucose levels
- Rapid decline: catecholamine release causing weakness, hunger, and tachycardia
- Slow decline: neurologic signs
- Clinical signs usually intermittent but become more frequent as the tumor progresses
- Poor correlation between feeding and onset of clinical signs
- Paraneoplastic peripheral polyneuropathy has been described in dogs with insulinoma with a clinical presentation of severely depressed to absent spinal reflexes (worse in the thoracic limbs) and extensive axonal degeneration
- Hypoglycemia with a blood glucose concentration < 60 mg/dL
- Hyperinsulinemia with a blood insulin concentration > 20 μU/ml
- Diagnosis of insulinoma is based on demonstration of concurrent hypoglycemia with hyperinsulinemia:
- Glucose level and insulin assay from same blood sample (75% increased)
- Relative hypoglycemia calculated using:
- Insulin-to-glucose ratio > 0.23
- Glucose-to-insulin ratio < 3.31
- Amended insulin-to-glucose ratio > 30
- Amended insulin-to-glucose ratio = (insulin x 100) ¸ (glucose - 30
- Amended insulin-to-glucose ratio is the most sensitive test, but has poor specificity and false-positive results in dogs with liver disease, sepsis, and non-islet pancreatic tumors
- Other serum biochemical abnormalities include hypoalbuminemia, hypophosphatemia, hypokalemia, and increased ALP and ALT activity
- Low serum fructosamine is consistent with an insulinoma and has been reported in 1 dog
- Provocative tests are not recommended as they are time consuming, expensive, unreliable, high-risk, and do not improve diagnostic accuracy
- However, provocative tests have been recommend if insulinoma is suspected but hypoglycemia is not present
- Provocative tests include prolonged fasting, intravenous or oral Glucose tolerance tests, L-leucine tolerance test, glucagon tolerance test, and tolbutamide tolerance test
- Ultrasonography for pancreatic lesions (22%-69%) and metastatic lesions in adjacent organs
- Endoscopic ultrasound is used in humans and has been investigated in dogs with pancreatic disease with good visualization of pancreatic parenchyma (i.e., lobular structure, pancreatic duct, and vessels) except for tips of the pancreatic limbs
- Thoracic radiography does not identify pulmonary metastases
- Nuclear scintigraphy using radioactive labeled octreotide is sensitive for masses as small as 3 mm
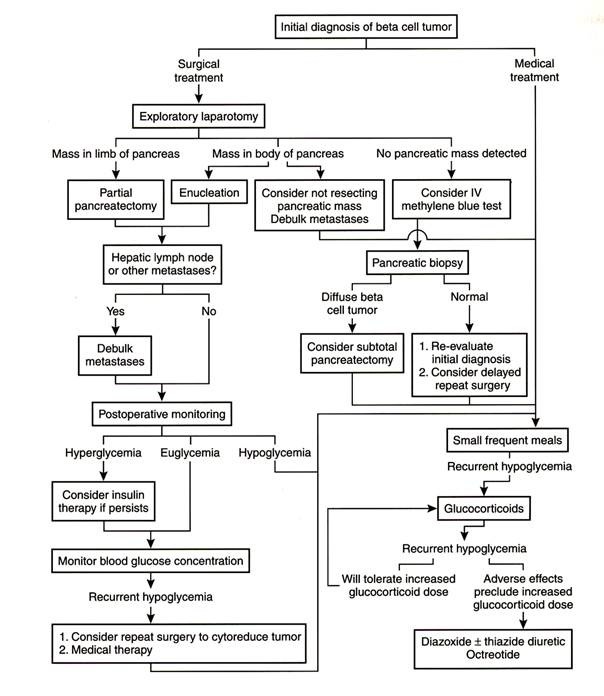
- Exploratory celiotomy
- Increased utilization of glucose with extrapancreatic neoplasms, sepsis, hunting dog hypoglycemia, polycythemia, and pregnancy
- Decreased production or availability of glucose with congenital or acquired hepatic failure, hypoadrenocorticism, puppy hypoglycemia, uremia, starvation, malabsorption, hypopituitarism, hypothyroidism, and glycogen storage disease
- Miscellaneous causes include insulin overdose and laboratory artifact
- 31%-51% have regional lymph node or liver metastasis at surgery
- Other metastatic sites include mesentery, omentum, duodenum, spleen, kidney, and spinal cord
- Metastasis to the lungs is rare
- Hypoglycemia is controlled with frequent feeding, reduced exercise, glucocorticoids, oral hyperglycemic agents, somatostatin analogues, and islet cell cytotoxic drugs
- Frequent feeds (4-6 times per day) with a diet high in protein and complex carbohydrates and low in simple sugars results in less stimulation of tumor-produced insulin and provide calories at frequent intervals
- Glucocorticoids (0.5-4.0 ml/kg/day) stimulate gluconeogenesis
- Prednisone ± diazoxide results in an improvement in clinical signs associated with hypoglycemia in 62% (8/13) dogs with conservatively managed insulinomas with a MST 74 days
- Diazoxide is a non-diuretic benzthiazide which increases blood glucose through several mechanisms:
- Inhibits insulin release from tumor cells by decreasing intracellular release of ionized calcium and blocking emiocytosis of insulin granules
- Stimulates hepatic gluconeogenesis and glycogenolysis by stimulating the sympathetic nervous system
- Decreases peripheral use of glucose both directly by inhibiting cellular uptake of glucose and indirectly by stimulating the release of adrenaline
- Augments free fatty acid mobilization
- Diazoxide is not an antineoplastic drug
- Diazoxide (5-30 mg/kg q 12 hrs) controls hypoglycemia in up to 59%-85% of dogs with mean response duration of 6.5 months (range, 2-15 months)
- Diazoxide effects may be potentiated by concurrent administration with another thiazide derivative hydrochlorothiazide (2-4 mg/kg q 12 hrs)
- Adverse reactions: anorexia, vomiting, and diarrhea
- Adverse reactions decreased by reducing dose and administering with food
- Glucagon CRI has been used as an emergency management of hypoglycemic-hyperinsulinemic crisis by achieving and maintaining normoglycemia despite intractable hyperinsulinemia
- Glucagon physiologically opposes actions of insulin by increasing hepatic glycogenolysis and gluconeogenesis
- Alloxan (65 mg/kg IV) is a derivative of uric acid which alters the permeability of pancreatic β-cells and causes permanent β-cell destruction resulting in prolonged hyperglycemia or normoglycemia
- Alloxan is toxic to renal tubular epithelial cells and causes renal failure in 10% dogs
- Streptozotocin and chlorozotocin have antineoplastic activity against islet cells
- Streptozotocin (500 mg/m 2 q 3 weeks) has been reported in 17 dogs with stage II and III insulinomas with prolonged median duration of normoglycemia compared to control dogs (163 days v 90 days) and resolution of paraneoplastic peripheral neuropathy in 2 dogs
- Acute and potentially fatal nephropathy, but aggressive saline diuresis during administration prevents nephrotoxic effects in dogs with reported toxicities including vomiting during administration, increased ALT activity which normalized after treatment was stopped, and azotemia in 1 dog
- Octreotide is a potent inhibitor of growth hormone, insulin, glucagon, and gastrin and has been used successfully in humans with hypoglycemia secondary to insulinoma but has no effect on circulating glucose and insulin levels in dogs with insulinoma
- Preoperative management depends on severity of hypoglycemia and other clinical signs
- Diet: high protein and complex carbohydrates fed 3-6 times daily
- Avoid semi-moist diets high in simple sugars
- Prednisolone or diazoxide for further stabilization if required
- 5%-10% dextrose solution intravenously if severe hypoglycemia and neurologic signs
- Approach: ventral midline celiotomy
- Insulinoma is usually solitary (79%), but can be multiple (18%) or diffuse (3%)
- Pancreas gently palpated for small nodules (< 1.0-1.3 cm diameter), but 3%-20% are not palpable
- Palpation of pancreas is unreliable when the tumor located in the head of the pancreas
- Tumor location has a relatively equal distribution between the left (44%) and right pancreatic limbs (35%)
- Rare sites include ectopic locations in the duodenal wall, diffuse non-palpable tumors, and tumors located in the body or head of the pancreas
- 45%-51% have regional lymph node or liver metastasis at surgery
- Tumor identification aided by:
- Intraoperative ultrasound (which is used very successfully in humans with pancreatic insulinomas)
- Intravenous 1% methylene blue (3 mg/kg diluted in 250 ml 0.9% sodium chloride and administered over 30-40 minutes), but hemolytic anemia due to Heinz body formation is a complication
- Partial pancreatectomy of left or right limb not recommended due to equal distribution of insulinoma
- Surgical techniques include enucleation, partial pancreatectomy (preferred), and total pancreatectomy
- Postoperative complications included pancreatitis, persistent hypoglycemia, hyperglycemia and diabetes mellitus, pancreatic pseudocyst, acquired epilepsy unrelated to hypoglycemia, and diffuse polyneuropathy
- Pancreatitis occurs in up to 10%-43% dogs and is treated with nil per os 36-48 hours and intravenous fluids
- Pancreatitis is common following resection of insulinomas located in the head of the pancreas
- Persistent hypoglycemia occurs in 15%-26% dogs due to inoperable or metastatic insulinoma
- Diabetes mellitus occurs in 8%-35% dogs due to prolonged hyperinsulinemia and hypoglycemia causing atrophy of normal islet tissue and partial pancreatectomy further decreasing insulin reserves
- Hyperglycemia is usually transient but can be permanent
- Epilepsy due to organic brain damage caused by recurrent severe hypoglycemia
- 12% (3/26) postoperative mortality rate because of pancreatitis or sepsis and diabetic ketoacidosis
- Prognosis is variable but usually guarded as surgical cure is not expected
- Recurrent hypoglycemia in 52%-100% dogs with time to recurrence of 60 days
- MST 74 days for conservative management
- MST 381 days for partial pancreatectomy
- Poor prognostic factors include:
- Age with survival time significantly decreased in younger dogs
- High preoperative serum insulin levels
- Stage III insulinomas with MST < 6 months v 18 months for stage I and II disease
- Persistent postoperative hypoglycemia (MST 90 days v 680 days for normoglycemic dogs)
- Conservative treatment (MST 74 days v 381 days)
- Enucleation compared to partial pancreatectomy (mean survival time 11.5 months v 17.9 months)
- Clinical stage is also important for duration of normoglycemia following surgical resection as dogs with stage I insulinomas maintain normoglycemia for a median of 14 months v 1 month for dogs with stage II and III disease
 From: Withrow SJ & MacEwen EG (eds): Small Animal Clinical Oncology (3rd ed).
From: Withrow SJ & MacEwen EG (eds): Small Animal Clinical Oncology (3rd ed).
PANCREATIC INSULINOMA
Stages
| I | Insulinoma confined to pancreas | II | Insulinoma with metastasis to regional lymph node | III | Insulinoma with metastasis to distant organs |
From: Withrow SJ & MacEwen EG (eds): Small Animal Clinical Oncology (3rd ed).
Conservative Management
General Considerations
Diazoxide
Glucagon
Chemotherapy
Other Medical Management
Surgical Management
Preoperative Management
Exploratory Celiotomy
Complications
Prognosis
Diagnosis
Laboratory Findings
Provocative Tests
Imaging
Other Diagnostic Techniques
Differential Diagnoses
Clinical Staging



